Some factors can make someone vulnerable to mental illness whilst others act as stressors or triggers for an episode of mental illness.
It is also very important to think about the positive factors in a person’s life that make them less likely to have mental health problems or make it more likely that they will recover from an episode of mental illness. These are called protective factors.
Vulnerability – The factors that make an individual more vulnerable to mental illness include:
Psycho-social
- any kind of trauma as a child (including bullying, abuse, neglect, physical illness)
- living in a community that is not their place of origin
Biological
- family history of mental illness (a “genetic” vulnerability)
- poor childhood nutrition
Stressors and triggers – some stress can be a positive motivating factor to enable people to achieve their goals, such as studying for an exam.
However, stress can also contribute to mental health problems, particularly if there are many stressors or if the stress goes on for a long time. Stressors and other triggers of mental illness include:
Psycho-social
- relationship, money, family, school, work or housing problems
- bereavement or any other type of loss
- being a victim of crime, assault, abuse or bullying
- belief that one is under the power of witches
Biological
- physical illness e.g. HIV/AIDS, malaria
- use of drugs or alcohol
Coping skills – Different people ‘cope’ with stress in different ways. Helpful coping mechanisms include talking to family or friends about the stressful situation. Unhelpful coping mechanisms can perpetuate mental illness. Drinking alcohol, taking illicit drugs and social isolation are all unhelpful coping mechanisms.
Support and security - Being able to confide in others, feeling safe in your home, having financial security, fulfilling a meaningful role within the family or community are all protective factors that can prevent the onset of mental illness and promote recovery from an episode of mental illness.
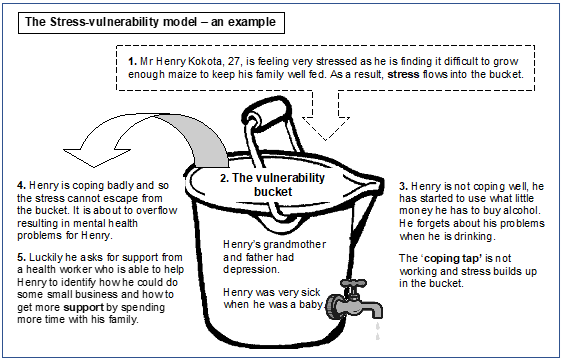
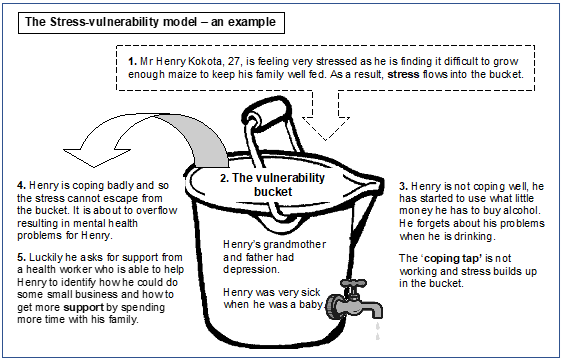
The Stress-vulnerability Model explains how vulnerability, stressors, coping and support interact to lead to mental health problems:
Vulnerability + stressors (+/- coping +/- support) = risk of mental health problem